Addiction Psychiatry
Judgment-free help for substance use and co-occurring mental health disorders. Manage cravings, empower sobriety, and get steady support that works.
We approach addiction as a chronic but treatable brain disease. There is no one-size-fits-all all plan. Whether you’re just starting on your recovery journey or you’ve been clean and sober for a while, we’ll meet you there. We treat withdrawal, cravings, and coexisting conditions. Our priority is a personalized, medical approach that helps you change your relationship with alcohol or other substances and improve your health.
You can expect:


Recovery is personal to each person. Whether you’re trying to cut down substances or live completely clean and sober, we’ll support your individual goals in the journey to a better life. Our licensed psychiatry team is experienced in assessing your unique symptoms and needs.
We’ve seen it all and can help get to the bottom of diagnosing clinical conditions and helping address addiction to:
We’ll take time to listen and translate a plan into easy-to-implement steps.

Find care that fits your needs.


We understand care shouldn't wait.
Get help from expert, specialized providers.
Schedule telehealth appointments at your convenience.
Accepting Medicare, Medicaid & commercial insurance.
We accept more than (20) insurance carriers - including Medicaid, TRI CARE, and most commercial insurance. Our goal? To bring quality psychiatry to all the Northwest, as affordably and accessibly as we can. To find out what your insurance will cover, contact us now for a complimentary benefits check.
No. Your goals guide the plan. Whether you want to start with harm reduction or are ready for full recovery, we’ll help you take that next step.
That depends on a few things. Often, success comes from a combination of medication, coaching, and community support. To decide what treatment plan is right for you, we’ll start with a careful evaluation and monitor your progress closely to make adjustments as needed.
Mental health conditions that exist in people struggling with substance misuse are called “co-occurring conditions.” You may also have heard this referred to as “dual diagnosis.” Either way, they are very common. And success in treating substance use often depends on treating your mental health conditions too. We treat them as the same time so nothing is missed, and you’re supported all around.
We’ll get you scheduled with the first available provider that fits your needs.
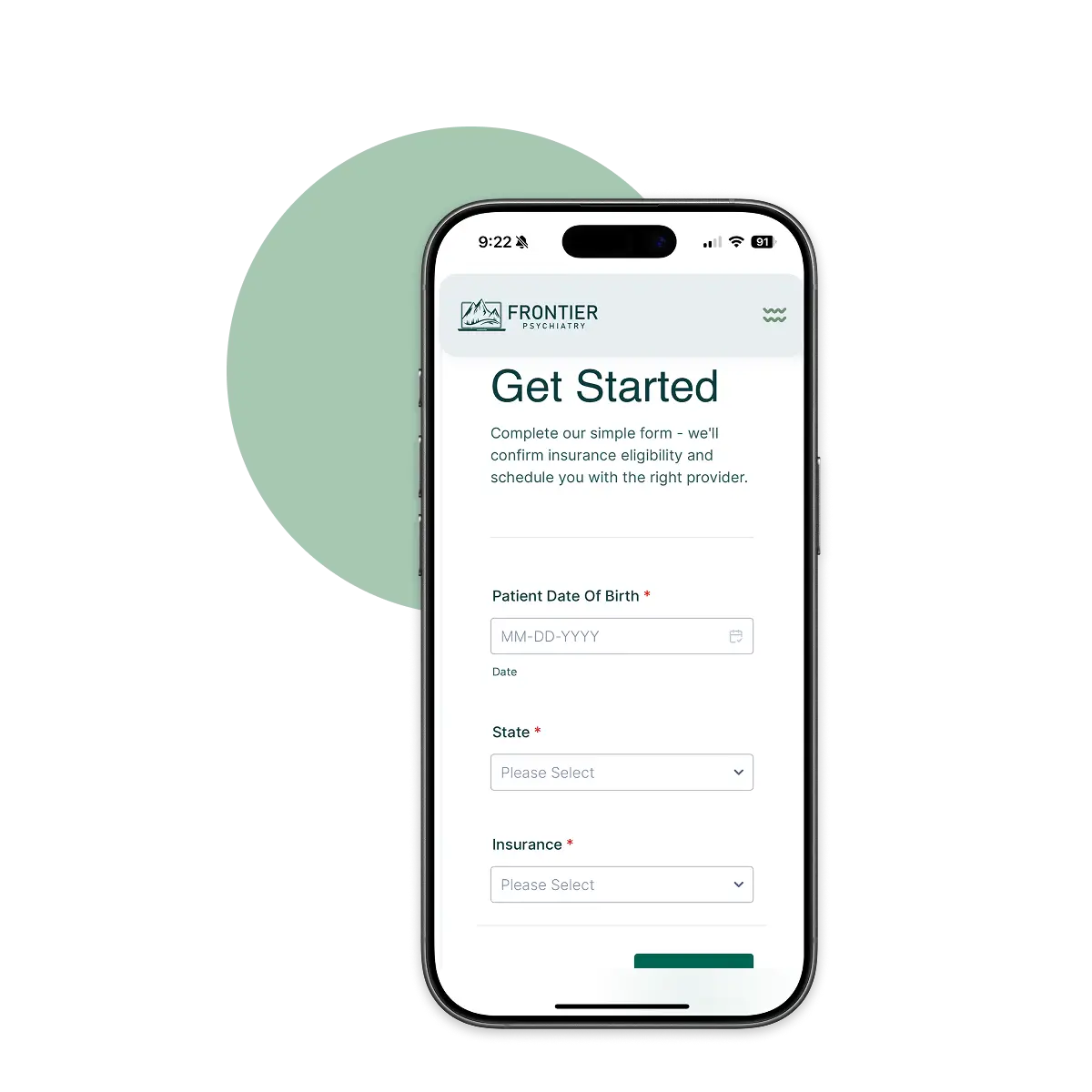
Get Started