If you’ve ever felt stuck in a cycle where using alcohol or drugs seems like the only way to cope with feelings of depression or anxiety, you are not alone. This frustrating tug-of-war between mental health and substance use is more common than you might think, and it has a name: dual diagnosis.
Dual diagnosis presents a complex health challenge, but it’s important to remember that what you’re experiencing is a legitimate medical condition rather than a personal failing. Understanding the links between addiction and mental health can allow you to break the cycle that may be dominating your life and create a strong foundation for genuine recovery.
What is Dual Diagnosis?
Dual diagnosis, also known as co-occurring disorders, is when an individual experiences both a mental health condition, like major depression, and a substance use disorder (SUD) simultaneously (1). One of the most challenging aspects of dual diagnosis is determining which condition came first. The truth is, this can be challenging to determine, and it is often more helpful to view these conditions as interconnected forces that mutually influence each other.
When Mental Health Leads to Substance Use
For many people who experience SUD, depression is a starting point. When the weight of sadness, anxiety, or hopelessness feels unbearable, you may find yourself turning to alcohol or drugs to find relief or self-medicate. The substance offers a temporary escape, a few hours of numbness or altered mood that provides relief from persistent emotional distress (2).
When Substance Use Triggers Mental Health Challenges
For others, substance use presents itself before mental health conditions. What might begin as recreational drug use can alter brain chemistry over time. The real-life consequences of addiction, such as strain on relationships, job loss, financial trouble, and feelings of shame, can serve as the perfect combination that causes a major depressive episode. In this case, the addiction itself can be the direct cause of the depression (2).
Why Co-Occurring Conditions Must Be Treated Together
Regardless of which condition came first, both are real, treatable, and need to be addressed together. Attempting to treat depression while still struggling with active addiction can feel like an uphill battle. On the other hand, achieving sobriety without tackling the underlying depression can create a higher risk for relapse. Healing requires a holistic approach that acknowledges this connection and treats the person as a whole, rather than focusing solely on isolated symptoms (1).
Biological Roots of the Depression-Addiction Connection
Depression and addiction are frequently linked due to underlying biology, genetics, and learned coping mechanisms. Understanding this can help remove the shame and blame that often surround these conditions, showing that this overlap is a recognized and treatable medical issue.
Shared Pathways in the Brain
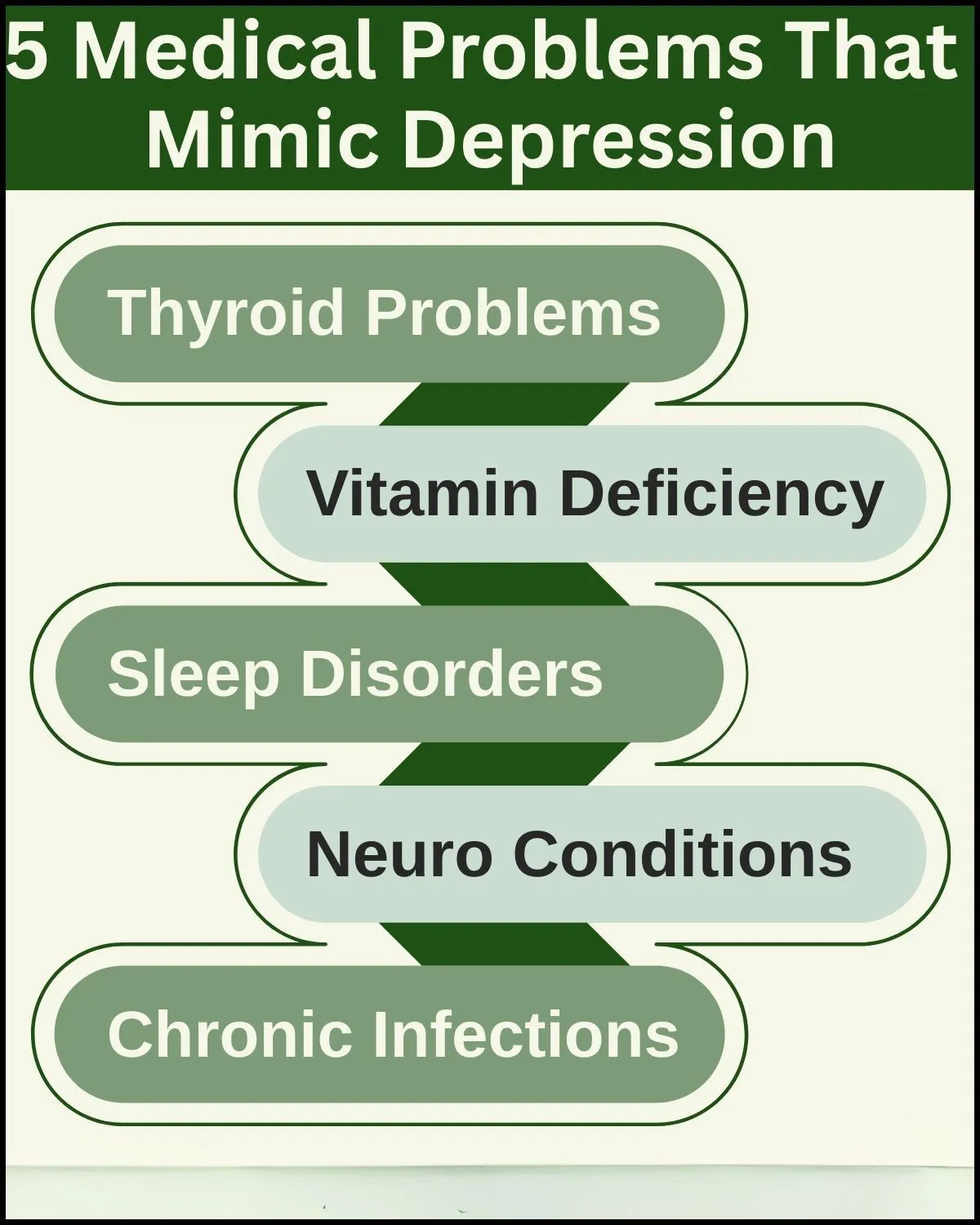
Mental health conditions and SUDs are related to imbalances in the brain’s chemistry. Your brain has a natural reward system that utilizes neurotransmitters like dopamine for pleasure and motivation, as well as serotonin for mood regulation. These neurotransmitters make you feel good during essential activities, such as eating or socializing.
With depression, this system is often underactive. This leads to anhedonia, or a loss of joy or enthusiasm for things you normally enjoy. When you use drugs or alcohol to cope, they artificially flood your brain with dopamine, creating powerful but false feelings of pleasure or reward.
Over time, the brain begins to rely on the substances you use, losing its ability to produce the “feel-good” neurotransmitters on its own. The result is a cycle where substances appear to be the only solution to the problem they helped create (3).
Underlying Risk Factors for Co-Occurring Disorders
Beyond brain chemistry, mental health conditions and SUDs often share root causes. Several key factors can increase a person’s risk for developing both conditions, including (3):
- Shared Genetic Predisposition: Certain genetic factors can influence how our brains process reward and manage stress, increasing risk to both depression and addiction.
- Overlapping Environmental Stressors: Experiences like chronic stress or trauma can alter brain development and stress responses, raising the risk for depression and increasing the likelihood of using substances as a coping mechanism.
- Impact on Similar Brain Circuits: Both conditions affect brain regions responsible for judgment, decision-making, and emotional regulation. Depression can weaken impulse control, making it harder to resist substances, while substance use further damages these circuits, worsening depressive symptoms.
The Trap of Alcohol and Depression
The relationship between mental health and SUD is perhaps most deceptive with alcohol. Because alcohol is legal and socially acceptable, it can seem like a harmless way to take the edge off a difficult day. Initially, alcohol may dampen anxiety or numb sadness.
However, alcohol is a central nervous system depressant, meaning it slows down vital functions like heart rate, breathing, and brain activity (6). This depressant action of alcohol explains the initial effects of relaxation and slurred speech.
5 Signs You’re in a Co-Occurring Disorder Cycle
If you are using alcohol to cope with depression, it can be hard to recognize when you are caught in the cycle. Here are five signs that may help you identify if you’re relying on coping mechanisms that are more harmful than helpful:
- Feeling the Trigger: Specific events or feelings can cause the overwhelming symptoms of depression or anxiety to spiral out of control.
- Seeking Escape: You drink alcohol to numb the emotional pain and quiet your mind.
- Physical Backlash: The alcohol disrupts your sleep cycle and depletes neurotransmitters like serotonin, which are crucial for mood stability.
- Intensified Crashes: You wake up feeling even more physically drained, emotionally fragile, and anxious than before.
- Stronger Cravings: The intensified negative feelings fuel a stronger urge to seek relief, pulling you back to alcohol and restarting the cycle.
If you see this pattern in your life, it does not mean you lack the willpower to break free. This cycle suggests that a powerful biological process is at work, and you may require support to overcome it.
Dual Diagnosis in Rural Areas: Challenges and Solutions
If you’re struggling with depression and SUD in a small town, you might encounter some challenges that city dwellers don’t face. Life in the countryside can be peaceful and community-focused, but the isolation can make it hard to find the support you need. Here are some obstacles you might run into (6):
- Scarcity of Care: Accessing care is often hindered by a lack of local options. Although you might find a nearby primary care doctor or counselor, specialized treatment centers for dual diagnosis are typically absent in remote areas. Traveling hours for a single appointment can feel like it’s not an option, especially when you’re already struggling with the exhausting symptoms of depression.
- Small Town Stigma: In a close-knit community, keeping your life private can be tough, and the stigma surrounding mental health and addiction is common. Many people worry about being seen entering a counselor’s office or treatment center, concerned about judgment from neighbors, their family’s reputation, or job security. This concern about public perception can cause many to keep their struggles hidden instead of seeking help.
- Practical Hurdles of Daily Life: Living in rural areas can make it hard to get regular medical treatment. Limited public transportation makes travel difficult for non-drivers, while many people experience financial constraints that make it hard to afford travel, take time off work, or cover treatment costs. As a result, some individuals must choose between working to support themselves and their families and prioritizing their health.
Connecting Rural Communities to Care That Works
Living in a rural area comes with particular challenges, especially when it comes to accessing mental health care. The good news is that there are now more available resources than ever.
One of the most promising options is teletherapy, which enables individuals to receive therapy remotely. Through secure video calls, you can now connect with mental health and addiction specialists no matter where you live, all from the comfort and privacy of your own home (6).
This new technology eliminates long travel times, protects your privacy by eliminating the need for in-person visits, and offers more flexible scheduling options. While it doesn’t solve every problem, telehealth is a big step toward making specialized healthcare more accessible to everyone.
Treatment for Co-Occurring Disorders
If you or a loved one is facing the challenge of a dual diagnosis, it’s completely normal to wonder where to start with treatment. The key is to tackle both struggles together, since they are closely connected and require a joint approach for lasting recovery (1).
Why Integrate Treatment for Depression and Addiction?
Integrated treatment is the most effective strategy for treating your co-occurring conditions. This approach involves a coordinated team, or at least providers who communicate closely, working with you on both your mental health and substance use at the same time (1).
Instead of being bounced around from one separate clinic to another, you’ll have a unified plan where all parts of your care work together. This integrated model improves treatment outcomes, including higher rates of recovery and better quality of life (2).
What Does Comprehensive Care Look Like?
An integrated treatment plan utilizes multiple therapeutic tools and is designed specifically for your needs. Specialized treatment plans usually include:
- Comprehensive Assessment
The first step is a thorough evaluation by professionals experienced in dual diagnosis. This step helps your care team understand the full scope of both conditions you’re experiencing, how they interact, which came first, and the impact they have on your daily life. A professional assessment ensures you receive a treatment plan that addresses the underlying causes of your co-occurring conditions (1). - Detoxification (If Needed)
For many people, the recovery process begins with detoxification. If your body is dependent on a substance, a medically supervised detox is essential to manage withdrawal symptoms safely. This process stabilizes you physically and prepares you to fully participate in the therapeutic work to come (1). Because withdrawal can be dangerous, detox should always be medically supervised. - Psychotherapy (Talk Therapy)
Therapy is the heart of long-term recovery. Several therapy modalities are particularly effective for dual diagnosis:- Cognitive Behavioral Therapy (CBT): This is the primary approach in dual diagnosis treatment. CBT helps you identify the negative thought patterns and behaviors that fuel both depression (or anxiety) and addiction. By learning to reframe these thoughts, you can develop healthier coping mechanisms, rather than turning to substances (2).
- Motivational Interviewing (MI): Change is hard, and ambivalence is a normal part of the process. MI is a collaborative, non-judgmental therapy style designed to strengthen your own personal motivation and commitment to your recovery goals (1).
- Dialectical Behavior Therapy (DBT): Beneficial for managing intense emotions and reducing self-destructive behaviors, DBT provides practical skills in mindfulness, distress tolerance, and emotional regulation. It can be a game-changer for those who feel overwhelmed by their feelings (2).
- Peer Support Groups
Living in a rural community can often leave you feeling isolated in your struggles. However, just like telehealth services, the internet offers a way to connect with additional support for addiction. While traditional 12-step programs can be beneficial, finding groups specifically for those with a dual diagnosis, such as Dual Recovery Anonymous (DRA), can be especially validating. - Connecting with others who understand exactly what you’re going through provides essential support, instills hope, and teaches accountability. Many of these groups hold meetings online, making it easier to reach out and connect with others, no matter where you are.
Looking Forward
Recovery is a journey, and it’s important to remember that every step you take is valuable, no matter how small. By embracing an integrated approach that cares for both your mind and body, you build a solid foundation for a healthier, more stable future.
The Role of Medication in Dual Diagnosis Treatment (MAT)
When your care team suggests medication for your recovery, you may have questions or wonder if medication is just a substitute for the substance you were using. However, Medication-Assisted Treatment (MAT) is a scientifically proven method that helps with the biological aspects of addiction. This treatment stabilizes your brain chemistry, providing a strong base for the therapy work you’ll do. MAT is a crucial part of treating co-occurring disorders effectively (1).
How Medication-Assisted Treatment Supports Healing
If you’re facing dual diagnosis, the stability provided by medication can set you up for success. It’s common for powerful cravings and withdrawal symptoms to dominate thoughts, making it difficult to focus on the mental health work you do in therapy. MAT addresses this directly by:
- Reducing Cravings: Medications like Naltrexone (used for both alcohol and opioid use disorder) work by reducing the intense urges to use and blocking the “high” (2).
- Creating a Foundation for Therapy: By calming the constant noise of addiction, MAT allows you to fully engage in therapy to address the root causes of depression or other mental health struggles.
A Combined Approach: MAT and Mental Health Medications
Effective treatment for co-occurring disorders often involves a tailored medication plan. A professional may prescribe a combination of:
- MAT medications for managing the substance use disorder.
- Antidepressants (like SSRIs) are used to directly alleviate symptoms of depression.
While medications sometimes require a process of trial and error, your psychiatrist will guide you until you find the best combination for you. These medications work together to help you build a comprehensive path toward recovery (1, 2).
Integrated Healing with Frontier Psychiatry
Understanding dual diagnosis is the first and most important step toward reclaiming your life. If you recognize your own experiences in these words, remember that what you’re facing is a treatable medical condition, not a personal failure. Healing requires a compassionate, integrated strategy that addresses both conditions as part of one whole person.
You do not have to navigate your journey alone. At Frontier Psychiatry, we specialize in providing evidence-based, integrated treatment for co-occurring disorders. Our team understands the unique challenges faced by members of our community, and we are committed to creating a safe, confidential space for harm reduction and recovery. Through a personalized combination of therapy, medication management, and supportive care, we will work with you to break the cycle and build a sustainable foundation for wellness.
If you are experiencing co-occurring mental health and substance use struggles and live in Idaho, Montana, Wyoming, or Alaska, your path to a healthier, more balanced life can begin today. Please reach out to our team for a confidential consultation today. You can also schedule an appointment with our provider matching tool or call/text (406) 200-8471. Our specialists understand what you’re going through and will always meet you with sensitivity and support.
References
- Cleveland Clinic. (2022, November 16). Dual diagnosis. Retrieved from https://my.clevelandclinic.org/health/diseases/24426-dual-diagnosis
- National Institute of Mental Health. (n.d.). Substance use and co-occurring mental disorders. Retrieved July 9, 2024, from https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health
- Roncero, C., Palma-Álvarez, R. F., Abad, A. C., Fuster, D., Peralta, G., & Corominas, M. (2024). The management of psychiatric disorders with comorbid substance abuse: An updated narrative review. Journal of Clinical Medicine, 13(4), 999. https://doi.org/10.3390/jcm13040999
- Rural Health Information Hub. (n.d.). Substance use in rural areas. Retrieved July 9, 2024, from https://www.ruralhealthinfo.org/topics/substance-use
- Substance Use in Rural Communities: Barriers to Integrated Medication-Assisted Treatment for Rural Patients With Co-occurring Disorders: The Gap in Managing Addiction. (2020). Psychiatric Services. Advance online publication. https://doi.org/10.1176/appi.ps.202000312
- Understanding depressants. (2023, October 31). Alcohol and Drug Foundation. Retrieved from https://adf.org.au/drug-facts/depressants/ u