Are We Overusing the Term ‘Treatment Resistant’?
Psychiatrists are overusing the term “treatment resistant”. It’s a sloppy and dangerous practice.
Imagine you’re a patient with severe depression who has tried two different treatments without feeling any better.
At your next visit, you see that your diagnosis has been changed to “treatment resistant” depression.
H. Paul Putman III, MD argues that attaching those two words to any psychiatric diagnosis erodes trust and hope among our patients.
Last week, he wrote an editorial titled “The Failed Concept of Treatment Resistance” in the journal Psychiatric Research and Clinical Practice.
There is no consensus definition of “treatment resistant”.
Over the last two decades, the use of this fraught label has grown and now affects up to 60% of all diagnoses. Second opinions reveal that two-thirds of those cases can be effectively treated.
Are we just giving up too quickly?
We owe it to our patients to dig deeper:
- Have we reached out to a colleague for a second opinion?
- Are there exacerbating factors we’re not considering?
- Have we looked beyond the standard, first-line treatments?
- Is there a strong therapeutic alliance between patient and clinician?
Medication adherence rates in psychiatry are notoriously low and patients rarely attend more than four psychotherapy visits.
We owe it to our patients to think creatively about boosting engagement. That’s our responsibility.
Calling a disorder “treatment resistant” doesn’t absolve us.
Looking beyond first-line treatments is especially challenging in our rural healthcare deserts.
It’s rare and refreshing to read a provocative article by an “insider” like Dr. Putman: he is a Distinguished Life Fellow of the American Psychiatric Association.
I’m grateful for his call to action.
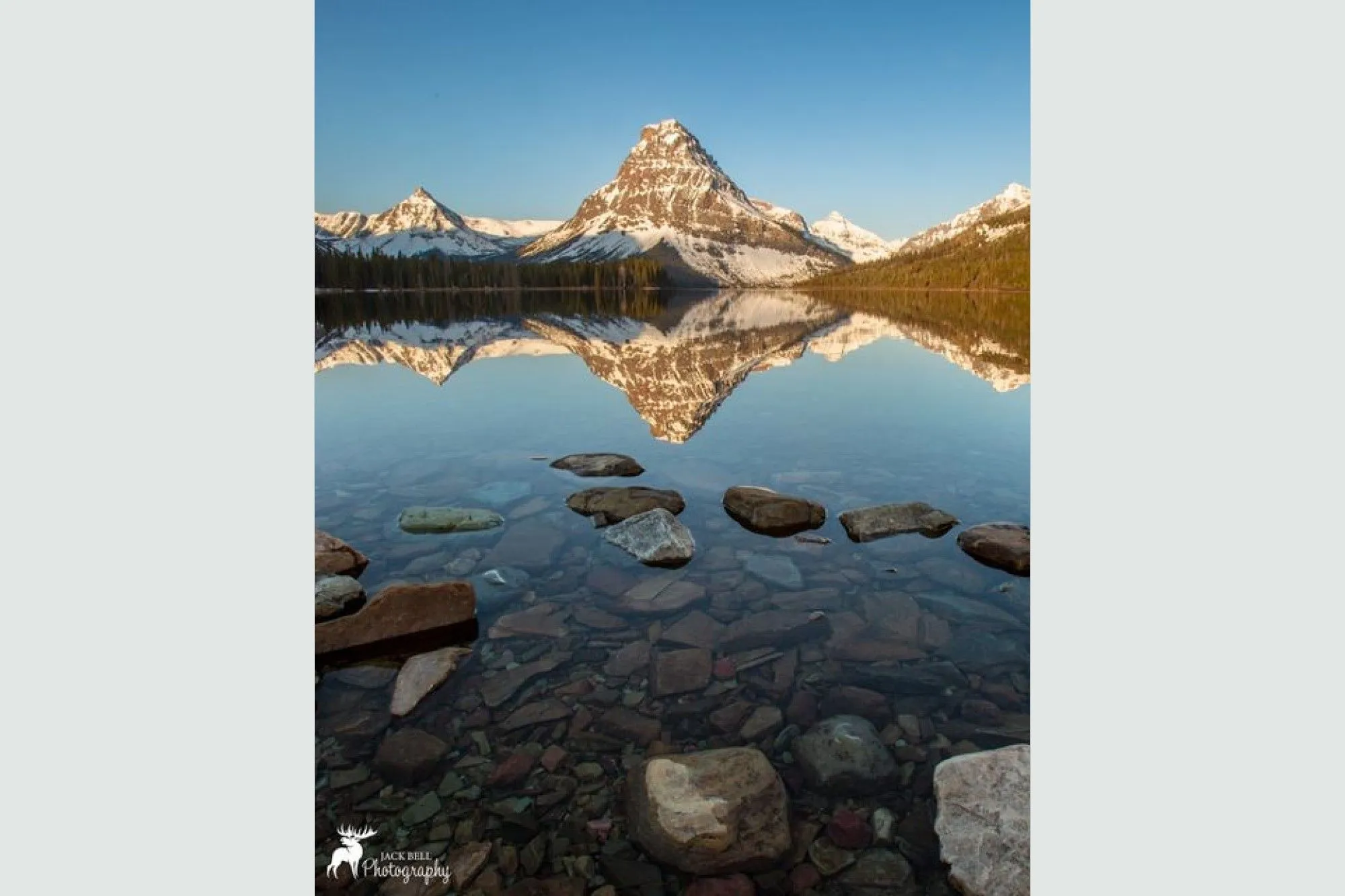
Photo Credit: Jack Bell Photography