The EmPATH Model in Action
In most hospital emergency rooms, psych patients in crisis have a pretty crappy experience.
There’s no excuse for that anymore.
They often wait days to be seen by a psychiatrist and get no care in the meantime.
Things are different at Centra Health in Lynchburg, VA.
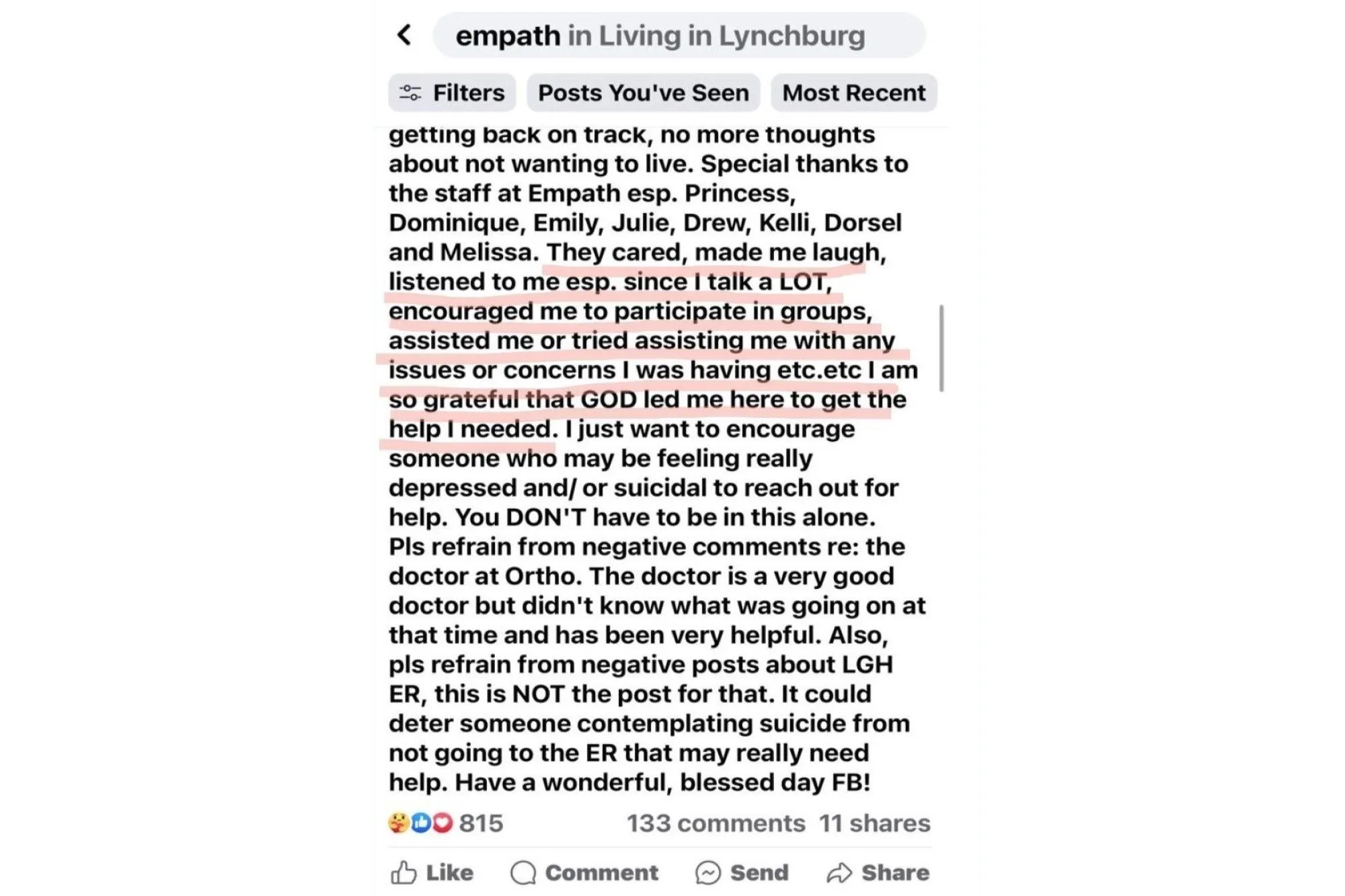
Their team is doing such a great job that a patient, after one of the worst days of her life, praised the staff publicly in a Facebook post on 11/3/23:
“They cared, made me laugh, listened to me esp. Since I talk a LOT, encouraged me to participate in groups, assisted me or tried assisting me with any issues or concerns I was having etc.etc.”
“I am so grateful that GOD led me here to get the help I needed.”
Yesterday, I spoke with Shannon Miles MSN, RN NEA-BC and Ismael Gama, MBA, MA, two leaders of Psychiatry & Behavioral Health at Centra Health in Lynchburg.
Last October, they led the opening of Virginia’s first-ever EmPATH unit, a model of behavioral health crisis care that is gaining traction nationally.
“EmPATH” stands for Emergency Psychiatric Assessment, Treatment and Healing.
Although I described my own experience with this model in an earlier post, I felt the need to tell another community’s EmPATH story to make a point.
Also, I think it’s time that we told more mental health care success stories.
Shannon and Ismael told me that patient care and satisfaction improved almost immediately.
Patients in crisis no longer had to wait 1-2 days to get care.
After just a few hours, patients were invited into the EmPATH unit where - right away - they received care from a nurse, a social worker, and an experienced nurse practitioner.
Before opening the EmPATH unit, over 80% of psych patients presenting to the ER had to be hospitalized.
Today, only 20% of patients need to be hospitalized. Accelerated access to care led to quicker stabilization of people in crisis.
Fewer hospitalizations meant more room in the hospital and fewer bottlenecks in the local system of care.
Why on earth isn’t this the standard of care nationally?
No, really. Why not??
So far, I think that the EmPATH unit is the best example of value-based care in behavioral health.
Deploying this model leads to better care, more efficient workflows, lower hospital admission rates, and a lower total cost of care.
We need more champions like Shannon and Ismael who act with a sense of urgency in service of our patients.
We also need fewer people in healthcare who automatically say “no” to common sense innovations in care delivery.
In June 2023, South Carolina’s Department of Health and Human Services committed $45.5 million to build 13 EmPATH units statewide.
That’s patient-centered leadership.